It will make your day
Posted by Bert Amaral on Tuesday, September 29, 2015
Monday, April 16, 2012
Rules for Being Human
Angels are everywhere if you only stop to notice. Sometimes, they even let you in on a few secrets.

Happiness consists of being perfectly satisfied with what we have, not with what we have achieved.
Rules for Being Human:

Happiness consists of being perfectly satisfied with what we have, not with what we have achieved.
Rules for Being Human:
YOU WILL RECEIVE A BODY
You may like it or hate it, but it will be yours for the entire period, at least this time around.
You may like it or hate it, but it will be yours for the entire period, at least this time around.
YOU WILL LEARN LESSONS
You are enrolled in a full time informal school called life. Each day in this school you will have the opportunity to learn lessons. You may like the lessons or think them irrelevant and stupid.
You are enrolled in a full time informal school called life. Each day in this school you will have the opportunity to learn lessons. You may like the lessons or think them irrelevant and stupid.
THERE ARE NO MISTAKES, ONLY LESSONS
Growth is a process of trial and error, experimentation. The “failed” experiment is as much a part of the process as the experiment that ultimately “worked”.
Growth is a process of trial and error, experimentation. The “failed” experiment is as much a part of the process as the experiment that ultimately “worked”.
A LESSON IS REPEATED UNTIL LEARNED
A lesson will be presented to you in various forms until you have learned it. When you have learned it, you can then go on to the next lesson.
A lesson will be presented to you in various forms until you have learned it. When you have learned it, you can then go on to the next lesson.
LEARNING LESSONS DOES NOT END
There is no part of life that does not contain it’s lessons. If you are alive, there are lessons to be learned.
There is no part of life that does not contain it’s lessons. If you are alive, there are lessons to be learned.
THERE IS NO BETTER THAN “HERE”
When your “there” has become a “here”, you will simply obtain another “there” that will again, look better than “here”
When your “there” has become a “here”, you will simply obtain another “there” that will again, look better than “here”
OTHERS ARE MERELY MIRRORS OF YOU
You cannot love or hate something about another person unless it reflects to you something you love or hate about yourself.
You cannot love or hate something about another person unless it reflects to you something you love or hate about yourself.
WHAT YOU MAKE OF YOUR LIFE IS UP TO YOU
You have all the tools and resources you need. What you do with them is up to you. The choice is yours.
You have all the tools and resources you need. What you do with them is up to you. The choice is yours.
YOUR ANSWERS LIE INSIDE YOU
The answers to life’s questions lie inside you. All you need to do is look, listen and trust.
The answers to life’s questions lie inside you. All you need to do is look, listen and trust.
YOU WILL FORGET ALL THIS
Unless you consistently stay focused on the goals you have set for yourself, everything that you have read won’t mean a thing.
— Anonymous Message from an Anonymous Angel
Unless you consistently stay focused on the goals you have set for yourself, everything that you have read won’t mean a thing.
— Anonymous Message from an Anonymous Angel
Monday, March 5, 2012
Care That Never Quits...
Pancreatic Cancer Prognosis
When your doctor gave you the initial pancreatic cancer prognosis, it may have erred on the side of caution. No one wants to give false hope, yet no one wants you to walk away from your initial pancreatic cancer prognosis feeling that there is no need to do anything further. Yes, the pancreatic cancer prognosis may be serious, however, the pancreatic cancer prognosis is not without hope.
At Cancer Treatment Centers of America one of the most valuable things we can give people who are dealing with a less than optimistic pancreatic cancer prognosis is hope. Call 800-487-3526 or click here to chat with on Oncology Information Specialist online about your pancreatic cancer prognosis. We can start you on the road to more effectively dealing with your pancreatic cancer prognosis.
Call 800-487-3526 and speak with an Oncology Information Specialist today. Healing and hope may be as close as a phone call. Your initial pancreatic cancer prognosis was not written in stone. You may have the power to change that prognosis for pancreatic cancer. Cancer Treatment Centers of America is ready to be your partner in making that change.
To Learn More About This Topic: Chat with Us | Email Us
Over Five Years Later:
A Survivor’s Story
When pancreatic cancer survivor Peggy was told there was no hope, she refused to give up and came to CTCA.
Conventional wisdom often says that the pancreatic cancer prognosis is not a good one. Conventional wisdom also says that cancer can't often be beaten, but we at Cancer Treatment Centers of America know that conventional wisdom can be wrong.When your doctor gave you the initial pancreatic cancer prognosis, it may have erred on the side of caution. No one wants to give false hope, yet no one wants you to walk away from your initial pancreatic cancer prognosis feeling that there is no need to do anything further. Yes, the pancreatic cancer prognosis may be serious, however, the pancreatic cancer prognosis is not without hope.
At Cancer Treatment Centers of America one of the most valuable things we can give people who are dealing with a less than optimistic pancreatic cancer prognosis is hope. Call 800-487-3526 or click here to chat with on Oncology Information Specialist online about your pancreatic cancer prognosis. We can start you on the road to more effectively dealing with your pancreatic cancer prognosis.
Pancreatic Cancer Prognosis: There is Hope
When you first received your pancreatic cancer prognosis, you most likely had a lot of questions. Some were as basic as "Will I survive?", others may have dealt with best treatment options, post treatment care, and life after treatment. At Cancer Treatment Centers of America we've dealt with all those questions and more. We are dedicated to giving you the most optimistic pancreatic cancer prognosis possible. We won't give you false hope, but we will give you hope. Hope that your initial pancreatic cancer prognosis can become brighter. Hope that your pancreatic cancer prognosis doesn't mean an end to life as you know it. Hope that, working together, we can find ways to bring health and healing to your initial pancreatic cancer prognosis.Call 800-487-3526 and speak with an Oncology Information Specialist today. Healing and hope may be as close as a phone call. Your initial pancreatic cancer prognosis was not written in stone. You may have the power to change that prognosis for pancreatic cancer. Cancer Treatment Centers of America is ready to be your partner in making that change.
What do you say to someone who is dying?
By Marsha Braddy
Heart of the Mountains Hospice
Talking to someone who is dying can be very uncomfortable. It can be so uncomfortable people often avoid, or want to avoid, visiting or talking with a dying person. People often state they “just don’t know what to say.”Heart of the Mountains Hospice
It is understandable we are at a loss for words around someone who is dying. We never wrote essays in school about talking to a dying person and dinner conversations don’t routinely cover this subject. It is especially difficult to find words when we are experiencing intense feelings of sadness and impending loss. We may only see their failing body, declining health, and vanishing spirit while losing sight of the fact a dying person is more than their death. Finding words in this painful situation necessitates a broader perspective than the moment we are in.
At any point in time a human being is a composite of their past, present and future.
Relating to people successfully includes referencing all three of these dimensions.
When we say “hello” to someone who is dying we need to be thinking about the person they were, the person they are, and the person they will become. When we ask “How are you?” we need to really mean it and not accept “fine” or “OK” as an answer. We need to say “No, I mean how are you really.” Then we need to listen and listen well, because talking with someone who is dying is as much about listening as it is about words.
We may not know much about the particulars a dying person shares such as diagnoses or tests or treatments. But we all know about pain, frustration, sadness, and loss. These feelings are not situation specific and we can say “I am so sorry you have to experience these things today.” Empathizing with someone who is dying is a powerful way to be with them. Even the dying person can only spend so much time with their decline and will need to move on.
You can say “I remember when things were different. Do you remember when we went fishing in that snowstorm?” or bring up some time in the past you were together. This can often be a comfortable time talking about your shared past and exchanging familiar remembrances that connect you in the world of memories. Talking about past experiences reminds everyone that the dying person’s life is more than what it is today.
When reminiscing is ending you can talk about tomorrow by asking “What will your tomorrow be like?” This question may take you into current events or it may take you into the final chapter of a life. When a dying person talks about “just waiting to go” you may squirm and say “I hate to hear you say that, my world will be different without you.” Tears and hugs and hand holding are meaningful because sharing emotions and touch are another powerful way to be with someone.
Ending a conversation or visit with a dying person can be hard. You can say “I have to go now, I have enjoyed talking with you, I am thinking about you.” You may be overwhelmed with lots of other thoughts and emotions, but know you have made a positive difference by spending time with someone and their past, present, and future. And when the dying person can no longer talk, you can still communicate with them by sitting quietly at their side in silence, remembering their life is so much more than this moment.
Sunday, February 12, 2012
Gene linked to pancreatic cancer growth, U-M study finds
Inactivating Kras caused tumors to disappear, suggesting possible treatment target
-added 1/31/2012Ann Arbor - A mutant protein found in nearly all pancreatic cancers plays a role not only in the cancer's development but in its continued growth, according to a new study from University of Michigan Comprehensive Cancer Center researchers. The finding suggests a possible target for developing new ways to treat this deadly disease.
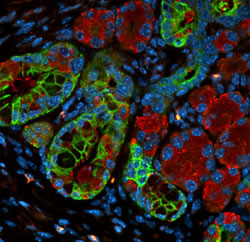
When Kras is turned off, early stage precancerous pancreatic lesions transform into normal pancreas cells.
Researchers have known that mutations in the Kras gene are what cause pancreatic cancer to develop. These mutations are frequently seen in common precancerous lesions, suggesting it has an early role in pancreatic cancer.
The new study, published in the February Journal of Clinical Investigation, finds that in mice, mutant Kras also keeps the tumor growing and helps precancerous tumors grow into invasive cancer. When the researchers turned off Kras, the tumors disappeared and showed no signs of recurring.
The researchers were able to manipulate Kras in a mouse model that they designed to look at Kras at various points in pancreatic cancer development. In the precancerous lesions, turning off Kras eliminated the tumors in mice and the pancreas tissue returned to normal, with no signs of the cancer returning. With invasive cancer, inactivating Kras killed off the cancer but left the pancreas with fibrous areas similar to scar tissue. Tumors did not recur.
Researchers hope this finding provides the basis for future drug development.
"Right now no drugs specifically target Kras, but there are drugs that target the cellular processes downstream of Kras. We next need to figure out which of these downstream effectors of Kras are important in pancreatic cancer," says study author Marina Pasca di Magliano, Ph.D., assistant professor of surgery and of cell and developmental biology at the U-M Medical School.
Kras is also known to play a role in lung and colon cancer. But it is likely the biggest player in pancreatic cancer, where more than 90% of all tumors have mutated Kras. Pancreatic cancer is one of the most deadly types of cancer: about 4% of patients are alive five years after their diagnosis. The disease is often diagnosed when surgery is not an option and it tends to be resistant to available chemotherapies.
"There is a dire need for new therapies for pancreas cancer based on a better understanding of the biology of this disease. My lab is now looking at the downstream inhibitors of Kras to try to find the best target," Pasca di Magliano says.
Note to patients: This research was based in mice and needs further testing before any possible treatments are available for clinical trials. For information about current pancreatic cancer treatments, call the U-M Cancer AnswerLine at 800-865-1125.
Pancreatic cancer statistics: 43,140 Americans will be diagnosed with pancreatic cancer this year and 36,800 will die from the disease, according to the American Cancer Society.
Additional authors: Meredith A. Collins, Filip Bednar, Yaqing Zhang, Jean-christophe Brisset, Stefanie Galban, Craig J. Galban, Sabita Rakshit, and Karen S. Flannagan, all from U-M; and N. Volkan Adsay from Emory University.
Funding: U-M Biological Scholar Program; National Cancer Institute; U-M Gastrointestinal Specialized Program of Research Excellence (SPORE); Pancreatic Cancer Action Network; American Association for Cancer Research; Michigan Gastrointestinal Peptide Research Center.
Disclosure: None
Reference: Journal of Clinical Investigation, Vol. 122, No. 2, February 2012.
Resources:
U-M Cancer AnswerLine, 800-865-1125 Pancreatic Cancer Clinical Studies
Cancer Clinical trials at U-M
Written by Nicole FawcettCancer Clinical trials at U-M
Monday, October 10, 2011
Battling the Effects of Cancer Treatments With a Fitness Plan
When faced with the issue of cancer treatment, many of the most difficult problems are the symptoms that may drag a person's energy levels down. However, it is very possible to combat negative treatment effects by exercising. A proper fitness routine has been shown to decrease stress levels while conditioning the body to have more stamina in those going through chemotherapy or radiation treatment. According to the American Cancer Society, chemical treatments have been known to cause side effects, both mental and physical in patients.
Exercise can allow cancer patients to increase overall energy, sleep more comfortably, and recover faster from treatments that may cause insomnia, lethargy, and mental havoc. Due to the inactivity commonly associated after a patient undergoes treatment, exercise can keep survivors active and help patients maintain a healthy weight. Prior to exercise, a complete physical should be done with a doctor to determine what type of fitness plan is appropriate. Factors, such as treatment options, disease prognosis, and current level of fitness are taken into account when creating an exercise plan. For those suffering with lung cancer or mesothelioma, a specific exercise plan must be created that does not cause additional complications to the respiratory system. This is why it is especially important to consult with a doctor when attempting to create an exercise plan.
Common effects of leukemic or mesothelioma treatment include irritability, fatigue, and reduced confidence. However, an exercise plan may help relieve some of these problems by reducing stress, increasing energy, and improving your mood. In addition, fitness plans allow you to become stronger, thinner, and fit while lowering the chances of developing heart disease. Other benefits include reducing the chance of diabetes and obesity. The American Cancer Society has also proven through research that recurrences of cancer can be kept to a minimum if a healthy diet and exercise are employed into the lifestyle of a patient that is doing chemotherapy or radiation treatment.
Exercise is not the cure for this deadly disease but it may help with other aspects of life that are common amongst cancer patients undergoing harsh treatments. Furthermore, the benefits of exercising weigh heavily in favor for cancer patients who seek a form of mental and physical relief during such a difficult time.
By: David Haas
Thursday, April 14, 2011
Go in peace: rituals for the dying.
JOYCE RUPP, O.S.M. is a spiritual director, retreat and conference speaker, and author of many books, including Praying Our Goodbyes (Ave Maria, 1988), Your Sorrow Is My Sorrow (Crossroad, 1999), and Walk in a Relaxed Manner (Orbis, 2005).
Much has been written about death and dying, particularly the stages of the process, including the physical, mental, and emotional responses accompanying end-of-life issues. There is much less information about how to attend spiritually to those entering the last days and hours of earthly life. How can we pray with the dying in a way that is supportive, caring, and respectful? How can we temporarily forgo the ache in our hearts as we focus on being a loving presence for them? Rituals can be a valuable source of support for the dying, but traditional church rituals are limited and those we do have often lack sufficient help for this significant transition.
I discovered the meagerness of these rituals on the day a dear friend died. That morning the nearness of impending death whispered in every corner of her house. Friends and family came and went in the crowded living room. They stood by the hospital bed, attempting to say farewell to the beloved woman in a semi-coma. As they did so, my heart felt the heaviness of each one's sorrow.
In that grief-laden atmosphere, my friend's sister-in-law approached me and whispered, "We ought to gather tonight and do some sort of ritual for Joan." I readily agreed, knowing how inept we all felt about telling her "goodbye." I agreed to plan a prayer service for that evening.
A combination of panic and dread collided in me as I drove home. My mind briefly reviewed the traditional rituals of the Roman Catholic Church. There was the Sacrament of the Anointing of the Sick, but this is usually given weeks or months preceding death. Even when the anointing is near the time of death, the sacrament is only allowed to be administered by a priest. Besides the fact I am not ordained, this ritual allows only minimal participation for those present (mainly observation and some brief responses to the prayers).
Non-ordained chaplains sometimes bless the dying with holy water, making the sign of the cross on the head, the mouth, the heart, the hands, and the feet. Other chaplains pray the litany of the saints. One hospital chaplain encourages those at the bedside of the dying to create their own litany by naming deceased family members and friends. In doing so, they are reminded that the one dying will soon be welcomed home by those who have gone before him or her. The rosary was another option that I knew to be of comfort to the dying.
Each of these Catholic rituals has value but none of them seemed to be what Joan and her family needed. Her loved ones needed a prayerful experience that would provide support and strength to Joan as she slowly slipped away, while also encouraging their own ability to peacefully let go of her.
To each his own
Knowing how to pray with others when death nears is difficult because what gives comfort and ease to one dying person can cause anxiety and unease for another. Such was the case when a beloved pastor of mine was dying. Although he was conscious, he could neither see nor speak. One of his priest friends and I stayed the night with him. At a moment when it appeared he was close to his last breath, his friend and I began singing church songs such as "Be Not Afraid" and "On Eagle's Wings."
As I gazed upon the pastor's face, I sensed the need for quiet, remembering what he had once told me about wanting silence in his house for his morning prayer. So I leaned down close to his ear and asked, "Would you like us to stop singing? If yes, squeeze my hand." His response, even in his weakened state, was to nearly squash my fingers!
Another time I was with a young man dying of AIDS who wanted the opposite of silence. He asked that classical music be played continually in his room during his final days. Because each person has his or her own needs when approaching death, we cannot presume that one or two church rituals will best assist every dying person.
Certainly what we do not want to do when we are at the bedside of the dying is to foist our own needs and beliefs onto the one who is departing. How unfair if we encroach on dying people's last moments, focusing on our own desires for consolation instead of centering on what will bring peace and serenity to them.
It helps greatly if those around the bedside know what the dying person appreciates about personal prayer. One family told me their father was completely inert and unresponsive as he lay dying. They decided to pray the Our Father because he always prayed it at home. As they began, he turned his head toward their voices and a faint smile appeared on his ashen face. The Our Father was obviously what resonated with him and brought consolation. They had chosen well.
Many times we do not know the patient's spirituality and can only guess at what he or she might need. No situation is ever the same. We learn as we observe and tend to the dying. We do the best we can, trusting our deepest intuition and our Spirit-connection to lead the way. I had been Joan's spiritual director for five years so I was familiar with how she prayed and what she valued but I knew of no satisfactory rituals I could use.
Silent presence
To calm my searching and clear my vision, I went for a walk in the woods. My feet plodded along while I struggled to think of something appropriate. I prayed intensely for guidance. Above me an owl with wide wings silently glided through the trees.
Then four deer stood not far from me, gazing with what seemed to be compassion in their eyes. Joan was passionate about nature and often found her comfort there. The sight of those creatures assured me I would find a ritual that would encourage her journey onward.
Memories of my time as a hospice volunteer surfaced. It was during my bedside times with the very ill that I discovered a new way to pray with them, a personal ritual allowing me to be present in a spiritual manner that was respectful of their own religion and way of praying.
As I sat in the presence of a hospice patient whose body was weakening, I sensed the soul expanding in freedom. It was as though the soul was "ripening," being readied for its journey onward, like an apple maturing toward its moment of departure from the tree. I saw myself as a privileged witness to this awesome event. Although I spoke very little, I did offer encouraging words, affirming the dying one's spiritual strength and ability to release the body's hold on life. Always I assured them they were not alone.
Occasionally I held a hand, touched an arm, swabbed dry lips with moisture, or placed a wet washcloth on a fevered head, but mostly my physical actions were few. It was my "inner action" that I consistently gave to the patient. I tried to be a peace-filled presence of compassionate love as I imagined Mary of Nazareth was with when he was dying on the cross. Very intently I continuously gathered the love of God in my heart and sent it to the dying person, surrounding him or her with as much compassionate courage and peace as possible.
While "sending love" may not seem like a ritual, it does have its elements of gesture (inward attentiveness) and repetition (intentional sending of love over and over). I never knew whether or not this inner ritual was of value until two days before a beloved cousin of mine died. On Saturday morning I sat in her hospital room as she lay sleeping and "sent love" to her. I left before she awoke and on Sunday when I returned she appeared more peaceful than usual. As I drew near her bed, she turned to me and said, "You were praying for me while I rested yesterday, weren't you?"
Blessing the body
For Joan, I trusted the benefits of my personal inner ritual but realized we needed a communal one, something external that everyone could participate in and that Joan could hear. Then I realized I had missed something essential:
I had discounted the body with so much focus on the soul.
The soul was ripening but so was her body as it weakened and prepared for its separation from the soul. Through Joan's 55 years of life her physical body had been her faithful companion and instrument for spiritual growth. Whatever ritual we prayed, her body would need to be included. Out of this realization, I created a prayer service with the central component being that of the blessing of loan's body.
That evening when family and friends gathered around the hospital bed we knew we were standing at the threshold of a powerful moment for our loved one. Joan barely moved. Her breathing was shallow and her body calm. As we began the ritual, I invited everyone to remember the presence of the Holy One in our midst. We needed this to give us hope and strength. We listened as some of Joan's favorite poems by Mary Oliver were read. Next I explained how we were going to bless and thank Joan's body for what it had done for her and for us.
We spoke directly to Joan as we blessed the various parts of her body (head, eyes, ears, hands, etc.). We recalled what her body had done for her and thanked her for how she had used that part of her body in some way as a gift to us.
For example, when I prayed a blessing for her head (the dwelling place of her brain and mind), several persons standing nearby placed their hands on her head. I mentioned how she influenced our lives by her beliefs, attitudes, and values, and thanked her for sharing her dreams and hopes with us. Then those around the bedside added personal ways her head had helped them. After each part of her body was blessed, the group spoke together to Joan: "You will always be a part of our hearts. Go in peace." We continued in a similar manner for the rest of her body.
Throughout the ritual, Joan's 80-year-old mother gently held her daughter's bare feet in her hands while loan's husband bent close by her side. When it came time to bless her womb in gratitude for the wonderful life it had carried within it, her two young-adult sons knelt down and put their heads on her stomach and cried, "Thank you, Mom! Thank you!"
During the entire blessing I stood at the back of the bed. We completed the farewell ritual by listening to a musical rendition of the Our Father that Joan had included in her funeral plans.
I'll never forget what happened after the music stopped. Throughout the blessing she had been silent and seemingly unaware of our presence. To our amazement, after the closing song she slowly raised her right arm and extended it backward toward me for a brief moment. Then the arm flopped down limply on the bed. Joan had heard everything and was trying to express her gratitude!
Healing at the end
Since that time, I have used the blessing in similar situations and have shared it with others who have waited with the dying. People continually assure me that it provides both their loved one and themselves with the surrender and peace they need.
A chaplain recently told me of a woman who clung to her husband's body after he died and could not bear to leave him. As she tried to console her, the chaplain remembered the blessing of the body. When the ritual was completed, the widow turned and whispered, "Now I can leave."
Another chaplain recently described how she was in the intensive care unit ministering to a family with hostile emotions toward one another. Some had not spoken to each other for years. They stood or sat silently in far corners from one another as they waited to hear the surgeon's prognosis. Eventually they learned their loved one was not going to live.
When the family was able to enter the ICU room to say their goodbyes, the chaplain invited them to join her in the same ritual I used with Joan. The chaplain said it was like a miracle. By the time the ritual was completed, the family began to speak to one another, then to hug each other and to cry. The ritual helped them release their old wounds. In expressing gratitude to their family member and encouraging him to go in peace, they rediscovered a center of love that united them again.
Death is a momentous journey that each of us will one day take. I hope we will have what we need spiritually in our final days and hours. Let us urge those in pastoral ministry and chaplaincy to create meaningful rituals for end-of-life situations. Let us search for prayerful ways to assist patients, and those who are with them, to say goodbye in a comforting way. What a magnificent gift for the dying if our church could be a catalyst of compassion and consolation for the great transition from this life to the Beyond.
Much has been written about death and dying, particularly the stages of the process, including the physical, mental, and emotional responses accompanying end-of-life issues. There is much less information about how to attend spiritually to those entering the last days and hours of earthly life. How can we pray with the dying in a way that is supportive, caring, and respectful? How can we temporarily forgo the ache in our hearts as we focus on being a loving presence for them? Rituals can be a valuable source of support for the dying, but traditional church rituals are limited and those we do have often lack sufficient help for this significant transition.
I discovered the meagerness of these rituals on the day a dear friend died. That morning the nearness of impending death whispered in every corner of her house. Friends and family came and went in the crowded living room. They stood by the hospital bed, attempting to say farewell to the beloved woman in a semi-coma. As they did so, my heart felt the heaviness of each one's sorrow.
In that grief-laden atmosphere, my friend's sister-in-law approached me and whispered, "We ought to gather tonight and do some sort of ritual for Joan." I readily agreed, knowing how inept we all felt about telling her "goodbye." I agreed to plan a prayer service for that evening.
A combination of panic and dread collided in me as I drove home. My mind briefly reviewed the traditional rituals of the Roman Catholic Church. There was the Sacrament of the Anointing of the Sick, but this is usually given weeks or months preceding death. Even when the anointing is near the time of death, the sacrament is only allowed to be administered by a priest. Besides the fact I am not ordained, this ritual allows only minimal participation for those present (mainly observation and some brief responses to the prayers).
Non-ordained chaplains sometimes bless the dying with holy water, making the sign of the cross on the head, the mouth, the heart, the hands, and the feet. Other chaplains pray the litany of the saints. One hospital chaplain encourages those at the bedside of the dying to create their own litany by naming deceased family members and friends. In doing so, they are reminded that the one dying will soon be welcomed home by those who have gone before him or her. The rosary was another option that I knew to be of comfort to the dying.
Each of these Catholic rituals has value but none of them seemed to be what Joan and her family needed. Her loved ones needed a prayerful experience that would provide support and strength to Joan as she slowly slipped away, while also encouraging their own ability to peacefully let go of her.
To each his own
Knowing how to pray with others when death nears is difficult because what gives comfort and ease to one dying person can cause anxiety and unease for another. Such was the case when a beloved pastor of mine was dying. Although he was conscious, he could neither see nor speak. One of his priest friends and I stayed the night with him. At a moment when it appeared he was close to his last breath, his friend and I began singing church songs such as "Be Not Afraid" and "On Eagle's Wings."
As I gazed upon the pastor's face, I sensed the need for quiet, remembering what he had once told me about wanting silence in his house for his morning prayer. So I leaned down close to his ear and asked, "Would you like us to stop singing? If yes, squeeze my hand." His response, even in his weakened state, was to nearly squash my fingers!
Another time I was with a young man dying of AIDS who wanted the opposite of silence. He asked that classical music be played continually in his room during his final days. Because each person has his or her own needs when approaching death, we cannot presume that one or two church rituals will best assist every dying person.
Certainly what we do not want to do when we are at the bedside of the dying is to foist our own needs and beliefs onto the one who is departing. How unfair if we encroach on dying people's last moments, focusing on our own desires for consolation instead of centering on what will bring peace and serenity to them.
It helps greatly if those around the bedside know what the dying person appreciates about personal prayer. One family told me their father was completely inert and unresponsive as he lay dying. They decided to pray the Our Father because he always prayed it at home. As they began, he turned his head toward their voices and a faint smile appeared on his ashen face. The Our Father was obviously what resonated with him and brought consolation. They had chosen well.
Many times we do not know the patient's spirituality and can only guess at what he or she might need. No situation is ever the same. We learn as we observe and tend to the dying. We do the best we can, trusting our deepest intuition and our Spirit-connection to lead the way. I had been Joan's spiritual director for five years so I was familiar with how she prayed and what she valued but I knew of no satisfactory rituals I could use.
Silent presence
To calm my searching and clear my vision, I went for a walk in the woods. My feet plodded along while I struggled to think of something appropriate. I prayed intensely for guidance. Above me an owl with wide wings silently glided through the trees.
Then four deer stood not far from me, gazing with what seemed to be compassion in their eyes. Joan was passionate about nature and often found her comfort there. The sight of those creatures assured me I would find a ritual that would encourage her journey onward.
Memories of my time as a hospice volunteer surfaced. It was during my bedside times with the very ill that I discovered a new way to pray with them, a personal ritual allowing me to be present in a spiritual manner that was respectful of their own religion and way of praying.
As I sat in the presence of a hospice patient whose body was weakening, I sensed the soul expanding in freedom. It was as though the soul was "ripening," being readied for its journey onward, like an apple maturing toward its moment of departure from the tree. I saw myself as a privileged witness to this awesome event. Although I spoke very little, I did offer encouraging words, affirming the dying one's spiritual strength and ability to release the body's hold on life. Always I assured them they were not alone.
Occasionally I held a hand, touched an arm, swabbed dry lips with moisture, or placed a wet washcloth on a fevered head, but mostly my physical actions were few. It was my "inner action" that I consistently gave to the patient. I tried to be a peace-filled presence of compassionate love as I imagined Mary of Nazareth was with when he was dying on the cross. Very intently I continuously gathered the love of God in my heart and sent it to the dying person, surrounding him or her with as much compassionate courage and peace as possible.
While "sending love" may not seem like a ritual, it does have its elements of gesture (inward attentiveness) and repetition (intentional sending of love over and over). I never knew whether or not this inner ritual was of value until two days before a beloved cousin of mine died. On Saturday morning I sat in her hospital room as she lay sleeping and "sent love" to her. I left before she awoke and on Sunday when I returned she appeared more peaceful than usual. As I drew near her bed, she turned to me and said, "You were praying for me while I rested yesterday, weren't you?"
Blessing the body
For Joan, I trusted the benefits of my personal inner ritual but realized we needed a communal one, something external that everyone could participate in and that Joan could hear. Then I realized I had missed something essential:
I had discounted the body with so much focus on the soul.
The soul was ripening but so was her body as it weakened and prepared for its separation from the soul. Through Joan's 55 years of life her physical body had been her faithful companion and instrument for spiritual growth. Whatever ritual we prayed, her body would need to be included. Out of this realization, I created a prayer service with the central component being that of the blessing of loan's body.
That evening when family and friends gathered around the hospital bed we knew we were standing at the threshold of a powerful moment for our loved one. Joan barely moved. Her breathing was shallow and her body calm. As we began the ritual, I invited everyone to remember the presence of the Holy One in our midst. We needed this to give us hope and strength. We listened as some of Joan's favorite poems by Mary Oliver were read. Next I explained how we were going to bless and thank Joan's body for what it had done for her and for us.
We spoke directly to Joan as we blessed the various parts of her body (head, eyes, ears, hands, etc.). We recalled what her body had done for her and thanked her for how she had used that part of her body in some way as a gift to us.
For example, when I prayed a blessing for her head (the dwelling place of her brain and mind), several persons standing nearby placed their hands on her head. I mentioned how she influenced our lives by her beliefs, attitudes, and values, and thanked her for sharing her dreams and hopes with us. Then those around the bedside added personal ways her head had helped them. After each part of her body was blessed, the group spoke together to Joan: "You will always be a part of our hearts. Go in peace." We continued in a similar manner for the rest of her body.
Throughout the ritual, Joan's 80-year-old mother gently held her daughter's bare feet in her hands while loan's husband bent close by her side. When it came time to bless her womb in gratitude for the wonderful life it had carried within it, her two young-adult sons knelt down and put their heads on her stomach and cried, "Thank you, Mom! Thank you!"
During the entire blessing I stood at the back of the bed. We completed the farewell ritual by listening to a musical rendition of the Our Father that Joan had included in her funeral plans.
I'll never forget what happened after the music stopped. Throughout the blessing she had been silent and seemingly unaware of our presence. To our amazement, after the closing song she slowly raised her right arm and extended it backward toward me for a brief moment. Then the arm flopped down limply on the bed. Joan had heard everything and was trying to express her gratitude!
Healing at the end
Since that time, I have used the blessing in similar situations and have shared it with others who have waited with the dying. People continually assure me that it provides both their loved one and themselves with the surrender and peace they need.
A chaplain recently told me of a woman who clung to her husband's body after he died and could not bear to leave him. As she tried to console her, the chaplain remembered the blessing of the body. When the ritual was completed, the widow turned and whispered, "Now I can leave."
Another chaplain recently described how she was in the intensive care unit ministering to a family with hostile emotions toward one another. Some had not spoken to each other for years. They stood or sat silently in far corners from one another as they waited to hear the surgeon's prognosis. Eventually they learned their loved one was not going to live.
When the family was able to enter the ICU room to say their goodbyes, the chaplain invited them to join her in the same ritual I used with Joan. The chaplain said it was like a miracle. By the time the ritual was completed, the family began to speak to one another, then to hug each other and to cry. The ritual helped them release their old wounds. In expressing gratitude to their family member and encouraging him to go in peace, they rediscovered a center of love that united them again.
Death is a momentous journey that each of us will one day take. I hope we will have what we need spiritually in our final days and hours. Let us urge those in pastoral ministry and chaplaincy to create meaningful rituals for end-of-life situations. Let us search for prayerful ways to assist patients, and those who are with them, to say goodbye in a comforting way. What a magnificent gift for the dying if our church could be a catalyst of compassion and consolation for the great transition from this life to the Beyond.
Wednesday, April 13, 2011
Monthly Aspirin Use Linked to Lower Pancreatic Cancer Risk
MONDAY, April 4 (HealthDay News) -- Taking aspirin even once per month, whether low-dose or full strength, appears to be associated with a marked drop in the risk of developing pancreatic cancer, new research reveals.
The findings, from a team led by Dr. Xiang-Lin Tan, a research fellow at the Mayo Clinic in Rochester, Minn., are slated for presentation Monday at the annual meeting of the American Association for Cancer Research, in Orlando, Fla.
"This provides additional evidence that aspirin may have chemoprevention activity against pancreatic cancer," Tan said in a news release from the association.
But, he cautioned, "the results are not meant to suggest everyone should start taking aspirin once monthly to reduce their risk of pancreatic cancer. Individuals should discuss use of aspirin with their physicians because the drug carries some side effects."
To explore the protective potential of aspirin, the investigators focused on 904 pancreatic cancer patients and just over 1,220 healthy individuals, all of whom were seen at the Mayo Clinic between 2004 and 2010.
All of the study participants were at least 55. Questionnaires were completed to assess aspirin use between the ages of 41 and 60, as well as the use of nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen.
Using aspirin at least once per month was linked to a significant drop in pancreatic cancer risk, the research team concluded, even after accounting for other factors that might affect the finding, such as body-mass index and smoking history.
Those who had once smoked but kicked the habit seemed to experience an even stronger protective effect with respect to aspirin use than those who had never smoked or those who continued to smoke, the study authors noted.
NSAID and acetaminophen use did not, however, have any noticeable impact on pancreatic cancer risk, the authors added.
Dr. Michael Choti, a professor of surgery and oncology with the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University in Baltimore, expressed little surprise with the findings.
"There have been other preclinical findings suggesting that there may be some role for aspirin in inhibiting carcinogenesis, including pancreatic carcinogenesis," Choti noted. "And in other cancers, such as colon cancer, aspirin use has been associated with a reduction in cancer risk."
However, "studies that are not randomized trials are fraught with biases," he cautioned. "Those taking aspirin for a variety of reasons, say for cardiac or other cancer-protective effects, may generally have a better lifestyle, smoke less, eat better, exercise more. So one cannot purely conclude from this kind of study as to whether they are finding a general association between people who take aspirin, or in fact a true causative effect," Choti pointed out.
"But it's very interesting," he added. "And certainly the cost and risk of aspirin use is quite low. And this is compelling evidence to suggest there is some benefit, and it's perhaps another reason to advocate the use of aspirin."
Because the study was presented at a medical meeting, the findings should be viewed as preliminary until they are published in a peer-reviewed journal.
-- Alan Mozes
 Copyright © 2011 HealthDay. All rights reserved.
Copyright © 2011 HealthDay. All rights reserved.
Specifically, taking full-strength aspirin once monthly was linked to a 26% reduction in the risk of pancreatic cancer. Taking low-dose aspirin, to reduce the risk of heart disease, was associated with an even greater drop (35% lower) in pancreatic cancer risk.
"This provides additional evidence that aspirin may have chemoprevention activity against pancreatic cancer," Tan said in a news release from the association.
But, he cautioned, "the results are not meant to suggest everyone should start taking aspirin once monthly to reduce their risk of pancreatic cancer. Individuals should discuss use of aspirin with their physicians because the drug carries some side effects."
To explore the protective potential of aspirin, the investigators focused on 904 pancreatic cancer patients and just over 1,220 healthy individuals, all of whom were seen at the Mayo Clinic between 2004 and 2010.
All of the study participants were at least 55. Questionnaires were completed to assess aspirin use between the ages of 41 and 60, as well as the use of nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen.
Using aspirin at least once per month was linked to a significant drop in pancreatic cancer risk, the research team concluded, even after accounting for other factors that might affect the finding, such as body-mass index and smoking history.
Those who had once smoked but kicked the habit seemed to experience an even stronger protective effect with respect to aspirin use than those who had never smoked or those who continued to smoke, the study authors noted.
NSAID and acetaminophen use did not, however, have any noticeable impact on pancreatic cancer risk, the authors added.
Dr. Michael Choti, a professor of surgery and oncology with the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University in Baltimore, expressed little surprise with the findings.
"There have been other preclinical findings suggesting that there may be some role for aspirin in inhibiting carcinogenesis, including pancreatic carcinogenesis," Choti noted. "And in other cancers, such as colon cancer, aspirin use has been associated with a reduction in cancer risk."
However, "studies that are not randomized trials are fraught with biases," he cautioned. "Those taking aspirin for a variety of reasons, say for cardiac or other cancer-protective effects, may generally have a better lifestyle, smoke less, eat better, exercise more. So one cannot purely conclude from this kind of study as to whether they are finding a general association between people who take aspirin, or in fact a true causative effect," Choti pointed out.
"But it's very interesting," he added. "And certainly the cost and risk of aspirin use is quite low. And this is compelling evidence to suggest there is some benefit, and it's perhaps another reason to advocate the use of aspirin."
Because the study was presented at a medical meeting, the findings should be viewed as preliminary until they are published in a peer-reviewed journal.
-- Alan Mozes
Pancreatic Cancer Drugs Sutent And Afinitor Recommended By FDA Advisory Committee
Sutent (sunitinib malate) and Afinitor (everolimus) were recommended for approval for the treatment of unresectable pancreatic neuroendocrine tumors, a rare type of pancreatic cancer - by the FDA Oncologic Drugs Advisory Committee. Patients with advanced pancreatic neuroendocrine tumors (pNET) have limited treatment options; no new drug has been approved in three decades. Unresectable means that it cannot be removed by surgery.
Pancreatic neuroendocrine tumors affect approximately 0.32 in every 100,000 people, a very rare type of cancer. Unlike other pancreatic cancers, which result in death within a few months, pNET generally grows more slowly. Approximately 95% of all pancreatic cancers are pancreatic adenocarcinomas.
Dr. Mace Rothenberg, senior vice president of Clinical Development and Medical Affairs, Pfizer Oncology Business Unit, said:
The Committee appeared to be more impressed with Novartis' everolimus (Afinitor), which received a unanimously favorable vote, compared to 8-2 in favor of Pfizer's sunitibib (Sutent), a tyrosine kinase inhibitor.
Everolimus, which already was approved for kidney cancer treatment by the FDA on March 30, 2009, will probably exceed sales of $1.3 billion in 2015, experts estimate. Sunitinib is also an existing kidney-cancer drug - it was approved for the treatment of renal cell carcinoma and imatinib-resistant gastrointestinal stromal tumor (GIST) on January 26, 2006. Everolimus is currently used as an immunosuppressant to prevent the body from rejecting transplanted organs.
The Data Monitoring Committee for the SUN 111 trial (for Sutent) recommended the halting of randomization for the study in interest of patient safety and also on data indicating a high probability the study would meet its primary endpoint - progression-free survival - if it were to carry on to the end date of the study. A final analysis showed that Sutent more than doubled progression-free survival.
Written by Christian Nordqvist
Copyright: Medical News Today
Pancreatic neuroendocrine tumors affect approximately 0.32 in every 100,000 people, a very rare type of cancer. Unlike other pancreatic cancers, which result in death within a few months, pNET generally grows more slowly. Approximately 95% of all pancreatic cancers are pancreatic adenocarcinomas.
Dr. Mace Rothenberg, senior vice president of Clinical Development and Medical Affairs, Pfizer Oncology Business Unit, said:
"We are encouraged by the panel's favorable review of sunitinib for the treatment of unresectable pancreatic NET. Following today's discussion, we will work closely with the FDA to ensure that it has all of the information that it needs to finalize its review. If approved in the United States, sunitinib would be a major advancement in the treatment of patients with pancreatic NET, a disease for which there remains a significant unmet medical need."Although the FDA Advisory Committee's recommendations are not binding, the Agency tends to go along with what their members advise. Earlier on in the day the Committee recommended that another drug, Afinitor (everolimus) also be approved for the same type of cancer.
The Committee appeared to be more impressed with Novartis' everolimus (Afinitor), which received a unanimously favorable vote, compared to 8-2 in favor of Pfizer's sunitibib (Sutent), a tyrosine kinase inhibitor.
Everolimus, which already was approved for kidney cancer treatment by the FDA on March 30, 2009, will probably exceed sales of $1.3 billion in 2015, experts estimate. Sunitinib is also an existing kidney-cancer drug - it was approved for the treatment of renal cell carcinoma and imatinib-resistant gastrointestinal stromal tumor (GIST) on January 26, 2006. Everolimus is currently used as an immunosuppressant to prevent the body from rejecting transplanted organs.
The Data Monitoring Committee for the SUN 111 trial (for Sutent) recommended the halting of randomization for the study in interest of patient safety and also on data indicating a high probability the study would meet its primary endpoint - progression-free survival - if it were to carry on to the end date of the study. A final analysis showed that Sutent more than doubled progression-free survival.
Written by Christian Nordqvist
Copyright: Medical News Today
Monday, March 7, 2011
When You Feel Sad
When You Feel Sad
by James E. Miller
Your sadness is real, yet it need not be final.
You have known deep joy before;
you can yet again.
And while your despair brings you pain,
it can also bring you wisdom and strength.
From it you will learn secrets about yourself,
and truths about others.
Through it you will experience the blessings of healing,
and the mysteries of life.
So listen to your despair
and allow it to lead you to greater fullness.
And always remember: you are not alone.
You are loved, whatever happens.
You have significance, whatever befalls.
For you are an unrepeatable act in God’s grand creation.
You are irreplaceable.
At this moment, your journey in life
is requiring of you great courage, often unseen by others.
Be strong in your persistence.
Be supple in your patience.
And know: despite your brokenness,
and somehow even because of it,
wholeness awaits you.
Despite what you have lost,
and somehow even because of it,
you stand to gain.
You hold the possibility of experiencing life
with a maturity, and a compassion, and an appreciation
you have never known before.
So be open.
Know that the life which flows through you
has been given you as a sacred gift.
Cherish that gift.
Nurture it.
Above all else, hallow the preciousness
of each passing moment that is yours,
for this is where the miracle of life resides,
and this is where you must go to find it.
Finally, remember that your destiny was predicted
by the writer of the Book of Job:
"You will forget your misery,
you will remember it as waters that have passed away.
And your life will be brighter than the noonday;
its darkness will be like the morning.
And you will have confidence,
because there is hope."
you will remember it as waters that have passed away.
And your life will be brighter than the noonday;
its darkness will be like the morning.
And you will have confidence,
because there is hope."
Larry Miller http://www.willowgreen.com/
This excerpt is from the conclusion to the Willowgreen videotape Listen to Your Sadness: Finding Hope Again After Despair Invades Your Life by James E. Miller.
Subscribe to:
Posts (Atom)

























